 While many of its health-related efforts have been shunted into Verily, Alphabet (the company formerly known as Google) actually made health-related moves across its business this year. From search engine updates to massive research studies to M&A, read on for a timeline of Alphabet subsidiaries’ biggest digital health moves this year.
While many of its health-related efforts have been shunted into Verily, Alphabet (the company formerly known as Google) actually made health-related moves across its business this year. From search engine updates to massive research studies to M&A, read on for a timeline of Alphabet subsidiaries’ biggest digital health moves this year.
January 26: Verily, Alphabet’s main healthcare subsidiary, kicked off the year with an $800 million capital infusion from Temasek, a Singapore-based investment company. Temasek took a minority stake in the company and nominated a member to the company's board. In an email to MobiHealthNews, Verily stressed that the funding raise didn't come out of a need for operating capital, but instead was about bringing on a strategic partner in Temasek.
March 10: DeepMind, the Google-owned artificial intelligence company, announced that it was developing a new technology similar to blockchain for secure tracking of patient health data. In a blog post, London-based DeepMind said its new Verifiable Data Audit project could be the first steps toward a "a service that could give mathematical assurance about what is happening with each individual piece of personal data, without possibility of falsification or omission.”
April 17: Verily debuted a new health-tracking wearable designed for use in a series of observational and longitudinal studies. With the aptly-named Study Watch – which is not available for consumer purchase – the Alphabet subsidiary aims to push new boundaries in the size, scope, and sophistication of wearable data-gathering.
April 20: Verily launched the long-awaited Project Baseline Study, a collaborative effort with Stanford Medicine and Duke University School of Medicine to amass a large collection of broad phenotypic health data in hopes of developing a well-defined reference of human health. Project Baseline aims to gather data from around 10,000 participants, each of whom will be followed for four years, and will use that data to develop a “baseline” map of human health as well as to gain insights about the transitions from health to disease. Data will come in a number of forms, including clinical, imaging, self-reported, behavioral, and that from sensors (including Study Watch) and biospecimen samples.
May 10: Dr. Thomas Insel, former director of the National Institute of Mental Health, left Verily after a little under two years to join the founding team at Mindstrong. The company is developing objective measures of brain function based on patterns of interaction with a smartphone. Digital biomarkers Mindstrong measures include processing speed, attention, memory, and executive function.
May 18: Former FDA Commissioner Robert Califf revealed in a blog post that he has taken a job at Verily, and has returned to professorial positions at Duke and Stanford. Califf is working on Verily’s Baseline study, an effort to collect baseline health data on 10,000 people over the course of four years.
June 22: DeepMind, the AI-focused, UK-based Google subsidiary, announced it would roll out its Streams app in a second hospital. The deployment of the app at Musgrove Park Hospital marks the start of a planned five-year rollout with the Taunton and Somerset NHS Foundation Trust.
July 10: An independent review panel looking into DeepMind flagged a number of privacy and security concerns related to the Streams app, APIs (which serve as the borders for DeepMind Health’s applications as well as those of others like the NHS), data storage, and security of apps and other processes during the development stage.
August 7: The University of North Carolina tapped Verily and MindStrong for an ambitious 19-site study of post-traumatic stress disorder. The study, called the Aurora Study, is funded by a $21 million NIH grant and aims to enroll 5,000 people. Aurora was launched in September 2016 and has sought private funding to supplement the NIH grant. It's just now bringing on partners, however, and beginning to recruit participants.
August 15: Alphabet acquired a small, Seattle-based startup called Senosis Health for an undisclosed sum. Senosis, which had only recently come out of stealth mode, may not be a company many have heard of, although its founder Shwetak Patel, a professor at the University of Washington and a visiting researcher at Microsoft, is better known. Patel received a MacArthur Genius Grant in 2011 and has previously sold his startup Zensi to Belkin, and the core technology of another startup, SNUPI, to Sears. According to Senosi's now-inactive website, the company has created three health apps which use the smartphone's built-in sensors to monitor different health biomarkers.
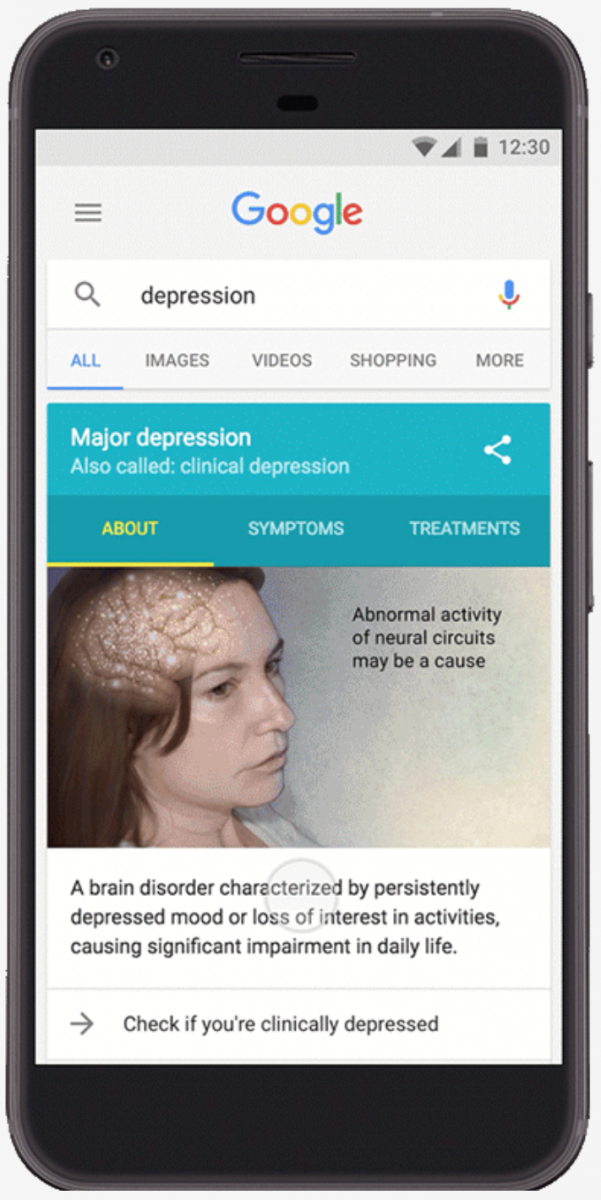
August 29: Through a partnership with the National Alliance on Mental Illness (NAMI), Google’s search engine began to direct people who search for clinical depression on mobile devices to a clinically-validated screening test (the PHQ-9) that can help them evaluate whether they might have the disease. When a user searches for "depression," a button labeled "Check if you're clinically depressed" will appear within the existing Knowledge Graph card. Pressing that button takes the user to the questionnaire (and an assurance that the data won't be stored). Based on the results, Google will offer a score on a scale of zero to 27, along with an interpretation of that score and advice on how to proceed. Severe scores include a direct link to the National Suicide Prevention Lifeline.
September 26: Verily was one of the nine companies announced in September as a participant in the FDA's new pre-certification program. The program could make it much easier for Verily to release certain kinds of health devices in the future.
October 1: Google’s Sidewalk launched Cityblock, a startup focused on reinventing urban health. Cityblock aims to address the health disparity in lower socio-economic urban communities by providing preventive medicine and access to resources.
October 3: Verily Chief Technology Officer Brian Otis took the stage at Health 2.0 to talk about all the company’s different efforts, using the metaphor of a car.
“If you do the math, there is basically ten orders of magnitude difference between the amount of data your car creates versus you,” Otis said at the time. “And ostensibly, as people, our bodies are more important than cars.”
October 17: Google briefly tested, but quickly removed, a feature in Google Maps that automatically added calorie counts to walking routes, and even expressed the number of calories as an equivalent number of “mini-cupcakes." The feature was rolled out on a test basis to some iOS users, but was rapidly panned on Twitter. In addition to a general feeling that the app was shaming or judgmental, individuals expressed concerns that it could have a negative effect on people with past or present eating disorders and that, because everyone's metabolism is different, the values were not usefully accurate. Users also pointed to the use of the (pink) mini-cupcake as offensively gendered.
November 27: In a proof of concept study, Google researchers described their experiences developing two automatic speech recognition methodologies for multi-speaker medical conversations, and concluded that both models could be used to streamline practitioners’ workflows. Researchers will begin working with Stanford University physicians and researchers to explore how technologies such as these can better lessen the burden on physicians.
November 29: A slew of digital diabetes care companies announced integrations with the upcoming virtual Type 2 diabetes management platform being developed by Onduo, a joint venture of Verily and Sanofi. These announced services include Voluntis’ Insulia, a digital insulin dose recommendation and coaching system; Glytec’s Glucommander Outpatient, cloud-based software that evaluates blood glucose and patient attribute to adjust insulin dosages; and BioTelemetry’s Telcare cellular-enabled glucometer and cloud-based data system.
December 5: As it did with depression in August, Google, through a partnership with the National Alliance on Mental Illness (NAMI) and the Department of Veterans Affairs’ National Center for PTSD, looked to increase the number of people with PTSD who seek help for their condition by conveniently surfacing an online version of the PC-PTSD-5 screening tool in response to certain search terms. The PC-PTSD-5 is intended to build awareness and improve linkage to care, but should not replace diagnosis from a professional.



















