 Last year the Essence Group raised $70 million in funding from investors that included Passport Capital, Camden Partners and Blue Cross Blue Shield Venture Partners. Essence is an umbrella organization, founded by venture capitalist John Doerr, that includes three healthcare companies: Essence Healthcareoffers people on Medicare a health plan that focuses on wellness, care coordination and personal service in six states; ClearPractice offers electronic health records; Lumeris is a supplier of analytic software that tracks procedures and patient results for insurers and physicians.
Last year the Essence Group raised $70 million in funding from investors that included Passport Capital, Camden Partners and Blue Cross Blue Shield Venture Partners. Essence is an umbrella organization, founded by venture capitalist John Doerr, that includes three healthcare companies: Essence Healthcareoffers people on Medicare a health plan that focuses on wellness, care coordination and personal service in six states; ClearPractice offers electronic health records; Lumeris is a supplier of analytic software that tracks procedures and patient results for insurers and physicians.
This week it seems Essence found a way to spend some of the millions it raised last year. Through its subsidiary, Lumeris, Essence teamed up with three other health plans, Highmark, Horizon Blue Cross Blue Shield of New Jersey, and Independence Blue Cross, to acquire provider and insurance real-time transactions network provider NaviNet for an undisclosed price. The deal should be final within 30 days, according to the companies.
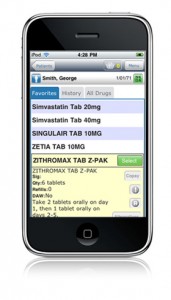
In 2010 NaviNet moved away from the desktop extended its offering into the exam room by acquiring mobile-enabled e-prescribing company Prematics. At the time of the acquisition Prematics only had 4,000 physician users and its service was only available for iOS devices and Windows Mobile devices. In 2010 NaviNet claimed that about 70 percent of US physicians plus hundreds of thousands of clinicians and other healthcare professionals in the US used NaviNet to access real-time clinical information from health plans, the company stated at the time.
Here's how NaviNet described its offering after the Prematics acquisition: “As a result, when physicians are in the exam room prescribing medications via handheld device, they can also use the device to receive information about generic or alternative drugs; submit real-time authorizations; and view benefits information in real time to determine patient financial responsibility,” according to the company's 2010 press release.
Now that NaviNet is set to become a bundled offering with Lumeris' accountable care organization platform, the companies expect to power the ACOs offered by health plans across the US: "All over the nation, health plans, including Highmark, Horizon, and IBC, are developing new value-based payment models that reward physicians for highly coordinated, high-quality accountable care. The integration of NaviNet and Lumeris' capabilities would allow plans to develop next generation accountable care delivery systems to contain costs and improve quality, while continuing to handle administrative transactions easily and cost-effectively," according to the press release this week.
One of the other Essence Group subsidiaries, ClearPractice, offers an EHR called Nimble that was specifically developed for Apple iPad users. ClearPractice offers Eden, a cloud-based EHR offering that works across Apple iOS devices and Mac computers — iPhones, iPads, MacBooks and Apple PCs.
The New York Times has a great writeup on the Lumeris-NaviNet deal here.
For more from the press release, read the full announcement below:
BOSTON, MA, Feb 14, 2012 -- Three of the nation's leading Blue health plans that work with more than 70,000 physicians and hospitals to deliver care to more than 11 million people announced today they are partnering with health IT provider Lumeris Corp. to acquire NaviNet. NaviNet is the nation's largest real-time communication network for physicians, hospitals, and health insurers. Lumeris and the three Blues -- Highmark, Horizon Blue Cross Blue Shield of New Jersey (Horizon), and Independence Blue Cross (IBC) -- have signed an agreement to acquire NaviNet for an undisclosed price. The transaction is expected to close within 30 days, subject to customary closing conditions.
The partners believe that fully collaborative relationships among physicians, hospitals, insurers, and patients are essential to increase the quality of care, lower costs, and increase patient and clinician satisfaction in the U.S. health care system. The partnership will build on NaviNet's best-in-class network for transactions among health care providers and insurers by launching an unprecedented initiative to deliver critical information and applications to drive accountable, value-based health care. Today, NaviNet speeds and simplifies more than 50 kinds of administrative, financial, and clinical transactions among three-quarters of America's physicians, 3,800 hospitals, and dozens of the nation's largest health insurers, including Highmark, Horizon, and IBC. The acquisition will position NaviNet to expand the customers served by its real-time communications network.
Lumeris has created the health care industry's first accountable care delivery platform. Built in the cloud from its creation, this innovative solution provides enriched clinical data, financial information, and expertise to support new payment models that reward improved outcomes, enhanced patient safety, and increased physician and patient satisfaction, while lowering overall health care costs.
Through the new partnership, NaviNet will leverage its real-time communication network and Lumeris' accountable care delivery platform to ease the adoption of new accountable care models throughout the country. All over the nation, health plans, including Highmark, Horizon, and IBC, are developing new value-based payment models that reward physicians for highly coordinated, high-quality accountable care. The integration of NaviNet and Lumeris' capabilities would allow plans to develop next generation accountable care delivery systems to contain costs and improve quality, while continuing to handle administrative transactions easily and cost-effectively.
"Facilitating better care collaboration has been a huge focus for us and this acquisition clearly demonstrates that others share our vision and are willing to push it to the forefront. We're thrilled to be working alongside such industry leaders and look forward to collectively setting the standard for accountable care," said NaviNet's President and CEO Bradley J. Waugh.
NaviNet connects a network of 70,000 physicians and hospitals throughout the service areas of Highmark, Horizon, and IBC, as well as more than 75 percent of physicians in the U.S. Together, the partners are committed to providing physicians and hospitals with the tools and information they need to jointly manage better clinical outcomes and financial risk. However, the accountable care solutions will be available to all NaviNet customers, including insurers, hospitals, physicians, and other care providers.
"This accountable care solution will enable NaviNet's customers to serve as an information partner with physicians and hospitals, helping them facilitate all the administrative, clinical, and financial tasks necessary to deliver more accountable care," said Mike Long, CEO of Lumeris. "Physicians, their patients, and health plans will all benefit from this unprecedented initiative -- the largest in the country supporting the accountable care movement that is transforming the U.S. health care system."
Said IBC's President and CEO Daniel J. Hilferty: "Independence Blue Cross relentlessly focuses on raising the quality and lowering the cost of care that our members receive. But our nation's current health care system of fragmented and uncoordinated care results in poor communication, incomplete sharing of information, and inefficiency -- which undermines accountability.
"By building on NaviNet's success, this exciting, new collaboration can provide physicians and hospitals easy access to the information and tools they need to move into this new era of accountable care, which we are confident will bring greater satisfaction to our customers and their doctors," said Hilferty.
About NaviNet NaviNet, America's largest real-time healthcare communications network, securely links leading health plans, industry partners and the government to hundreds of thousands of physicians, clinicians and other healthcare professionals. More than 75 percent of the nation's physicians are enrolled in the NaviNet Network, which touches 121 million covered lives. NaviNet's care collaboration solutions and services for unified patient information management (UPIM) address the full lifecycle of healthcare data management by providing single-source access to patient-centric administrative, financial and clinical information to reduce costs, increase efficiencies and improve quality of care. For more information, or to sign up for NaviNet, please visit www.NaviNet.net or call 617-715-6000 or 800-805-7569.
About Lumeris Lumeris provides the information technology, guidance, and operational services necessary for health plans and hospitals to transform their organizations into high-performing accountable delivery systems. The company's revolutionary Accountable Delivery Platform integrates data from disparate systems across the continuum of care, provides complete visibility into the clinical and financial performance of the enterprise, and delivers applications and information to key stakeholders and providers at the point of thought. Lumeris was launched five years ago by a team of health care and technology leaders led by John Doerr, a leading venture capitalist who has launched some of the world's most successful companies, including Google, Amazon and WebMD. To learn more visit www.lumeris.com or call 1-888-LUMERIS.
About Independence Blue Cross Independence Blue Cross is the leading health insurer in southeastern Pennsylvania. Nationwide, Independence Blue Cross and its affiliates provide coverage to nearly 3.1 million people. For 74 years, Independence Blue Cross has offered high-quality health care coverage tailored to meet the changing needs of members, employers, and health care professionals. Independence Blue Cross's HMO and PPO health care plans have consistently received the highest ratings from the National Committee for Quality Assurance. Independence Blue Cross is an independent licensee of the Blue Cross and Blue Shield Association. Visit us at ibx.com. Like us on Facebook. Follow us on Twitter @ibx.
About Highmark Highmark, Inc., based in Pittsburgh, is an independent licensee of the Blue Cross and Blue Shield Association, an association of independent Blue Cross and Blue Shield plans. Highmark serves 4.8 million members in Pennsylvania and West Virginia through the company's health care benefits business and is one of the largest Blue plans in the nation. Highmark has 19,500 employees across the country. For more than 70 years, Highmark's commitment to the community has consistently been among the company's highest priorities as it strives to positively impact the communities where we do business. For more information, visit www.highmark.com .
About Horizon Blue Cross Blue Shield of New Jersey Horizon Blue Cross Blue Shield of New Jersey, the state's oldest and largest health insurer, is a tax-paying, not-for-profit health services corporation, providing a wide array of medical, dental, and prescription insurance products and services. Horizon BCBSNJ is an independent licensee of the Blue Cross Blue Shield Association, serving more than 3.6 million members with headquarters in Newark and offices in Wall, Mt. Laurel, and West Trenton. Learn more at www.HorizonBlue.com .
















