 IBM's Careflow software
IBM's Careflow software
At the Health 2.0 conference in Santa Clara, California, a slew of big data demoes kicked off Wednesday morning. They showed a handful of different ways data analytics can change healthcare -- whether the data comes from insurance claims or electronic health records. The theme was that big data didn't have to mean population data -- new initiatives are bringing the weight of large data sets to bear on individual patient cases.
Colin Hill, CEO and president of GNS Healthcare, displayed a project GNS is working on in partnership with Aetna. GNS's pilot used claims data and biometric screenings to do predictive analysis on patients at risk for metabolic syndrome or pre-diabetes. Hill said GNS's model is novel because the data is individualized, rather than population-based. That is, instead of merely analyzing aggregated data to find best practices, his team used data to determine which specific members of the population were most at risk for metabolic syndrome, and what factors were most likely to push them over the edge.
"When you can make it an individualized risk the chances of engagement go way way up," Hill said. "Pinpoint the specific information that will have the strongest bang for your buck."
GNS also created a rougher "first pass" version of the software with just the claims data, which Hill said was also effective. He said in the future, data sources like remote monitoring could further empower these kinds of models.
"The current medical system takes a single snapshot of a person once a year, twice a year," he said. "There's no reason continuous monitoring isn't something that becomes standard in a few years. The data is no longer the problem, it's not the bottleneck."
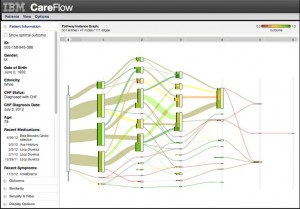
IBM Research Scientist Adam Perer showed off a program in development at the IBM research lab called Careflow. The software is for complicated patients -- ones that might have an unusual combination of co-morbidities. It searches the EHR for all other historic patients with the same combination of ailments and indications and then displays a decision tree-like graphic. Treatment paths are displayed as lines, with green lines representing treatments that minimized hospitalizations and red lines representing those that didn't. More popular treatment paths were displayed as thicker lines.
What Perer and his team found was that in some of these complicated situations, the most prescribed treatment path was not the one with the best history of good outcomes.
Charlie Wiggins, co-founder of Remedy Partners reported on a bundled payment pilot study Remedy recently ran. Bundled payments are one of the most radical approaches to value-based care: Medicare will give hospitals a flat payment per "episode of care". If the hospitals spend less than that, they share the savings. Spend more and they have to pay.
"In a bundle is everything that occurs with patients from the time they're admitted up to 90 days following discharge," Wiggins said. "CMS expects 2-3 percent savings per bundle."
Wiggins presented data about how payments were spent in the 425-patient pilot. He found that a large portion of each patients' bundle was actually spent outside the hospital in places like hospices and skilled nursing facilities.
"We've had some executives jump out of their chair when they see that about two thirds of spending in a bundle occurs outside of the hospital, and this is for both medical and surgical," he said. He suggested that nursing facilities are "not managing the patient condition, they're managing directly to the benefit."
Finally, healthcare data journalist and author Fred Trotter presented two new datasets from his DocGraph initiative. Trotter used Medicare data obtained via the Freedom of Information Act to put together data visualizations of physician referral networks and drug prescriptions. Again, some of the value of that data wasn't trends, but specific cases. He said that the data revealed some suspicious patterns of referrals that even resulted in doctors being fired for unethically referring or prescribing.
"Sometimes the dataset is showing very clear fraud, very clear partnerships," he said. "In general though, the amazing thing about this data set is a kind of analysis that I think is the future for our kind of work."

















