 An app that essentially elevates coughing into a smartphone into a sophisticated diagnostic tool has performed well again in a clinical study. Australian digital health company ResApp, which makes a smartphone-based tool for diagnosing respiratory conditions, reported 91 to 100 percent accuracy with the app in a study of 243 patients spanning six different respiratory conditions.
An app that essentially elevates coughing into a smartphone into a sophisticated diagnostic tool has performed well again in a clinical study. Australian digital health company ResApp, which makes a smartphone-based tool for diagnosing respiratory conditions, reported 91 to 100 percent accuracy with the app in a study of 243 patients spanning six different respiratory conditions.
The results are part of an ongoing study at Joondalup Health Campus and Wesley Hospital in Perth, Australia, using the ResApp diagnostic app. The app was developed from proprietary technology created at the University of Queensland with an initial grant from the Bill & Melinda Gates Foundation, and uses sound to diagnose respiratory conditions.
Previously, the company reported 89 percent accuracy for diagnosing respiratory diseases in a clinical study of 524 pediatric patients, and ResApp will soon launch a US pediatric study at three confirmed hospitals (so far, only Massachusetts General has been announced). The study will evaluate the ResAppDx software in the diagnosis of childhood pneumonia and other respiratory conditions.
ResApp’s product starts with a cough. The smartphone microphone acts as a stethoscope, but the app doesn’t need the well-trained ears of a doctor to form the diagnosis from those sounds – ResApp has been developing a machine-learning algorithm to do that job, diagnosing conditions including chronic obstructive pulmonary disease, pneumonia, asthma and upper respiratory tract infections.
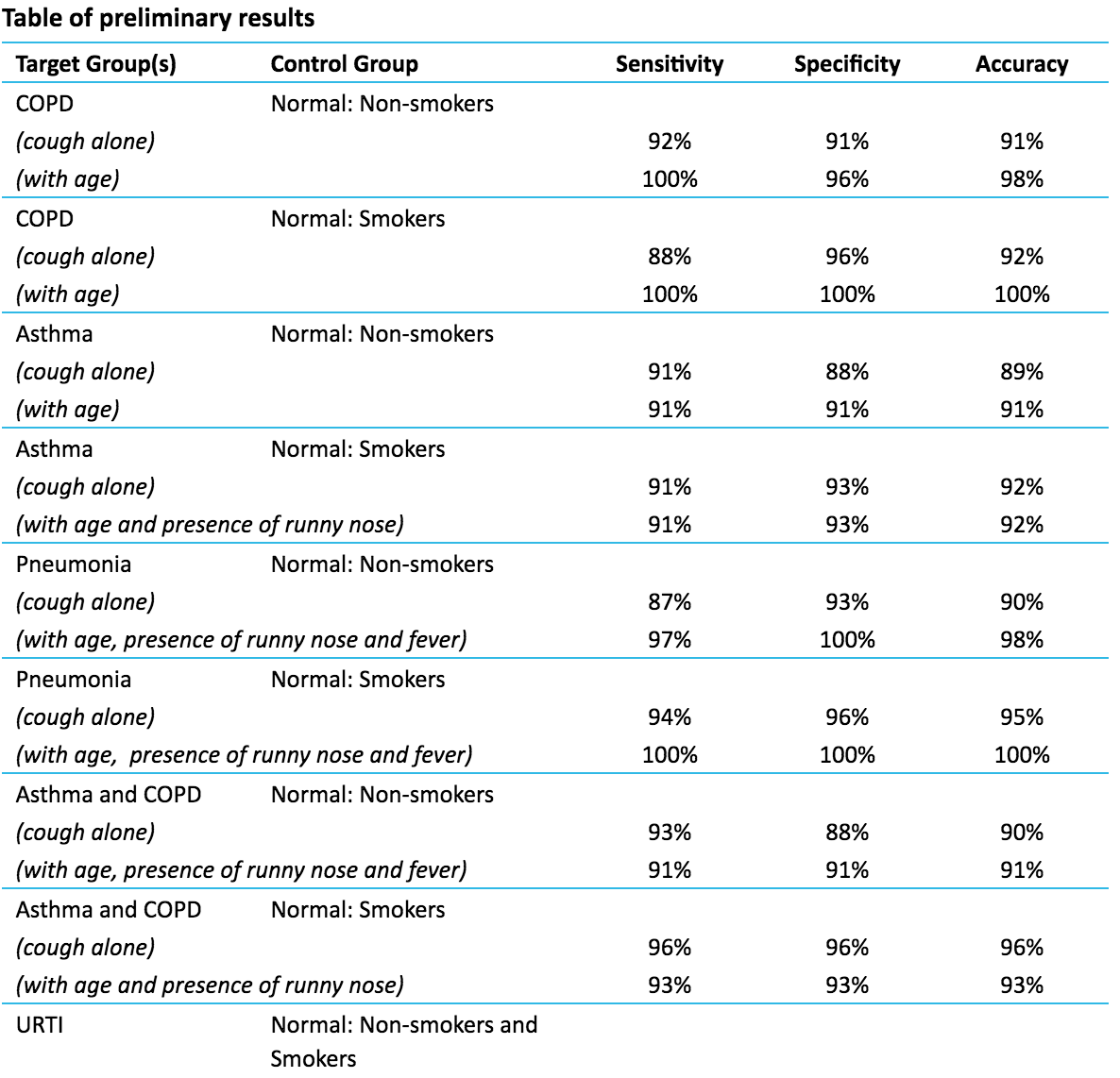
The cough sound-based algorithms were correct 91 to 100 percent of the time in distinguishing adult patients with COPD, asthma or pneumonia from subjects with no discernible respiratory disease, and demonstrated accuracy of 100 percent in distinguishing patients with an upper respiratory tract infection from those with no respiratory disease. Additionally, ResApp was able to able to correctly identify differential diagnosis of asthma versus COPD, pneumonia versus asthma, and pneumonia versus COPD in the range of 88 to 94 percent, the researchers reported.
Similar to the success of the previous study on pediatric patients, the algorithms were able to correctly identify lower respiratory tract disease in 84 percent of patients who were initially diagnosed as clear by real doctors using real stethoscopes (but were later found to have the diseases after additional clinical testing).
“We are pleased to again report high levels of accuracy in a significantly larger dataset, which continues to build our clinical evidence base as we progress toward an FDA submission,” Tony Keating, CEO and managing director of ResApp said in a statement. “It is also excellent to note that once again our algorithms outperformed experienced clinicians by correctly detecting lower respiratory tract infection in patients initially diagnosed as clear.”

















