
 Prescription digital therapeutics company Pear Therapeutics announced late last week that it has filed an FDA marketing authorization for Somryst, its digital cognitive behavioral therapy for the treatment of adults with chronic insomnia and depression.
Prescription digital therapeutics company Pear Therapeutics announced late last week that it has filed an FDA marketing authorization for Somryst, its digital cognitive behavioral therapy for the treatment of adults with chronic insomnia and depression.
While an approval from the agency would mark the third authorized prescription digital therapeutic for Pear — behind reSET for substance use disorder and reSET-O for opioid use disorder — the Somryst application is also the first product to CEO and President Dr. Corey McCann’s knowledge submitted through the FDA’s Precertification Program’s Working Model.
“We are a platform company really developing this whole new space of prescription digital therapeutics. We have the first two products that are market authorized by the FDA, and with this third you see a very strong commitment to developing a portfolio of products for serious disease,” McCann told MobiHealthNews. “And the second notable thing is we submitted this product via the FDA’s precertification pathway, and to my knowledge this is the first product submitted via that pathway. So in the spirit of developing a whole portfolio of these products, I think this is somewhat noteworthy.”
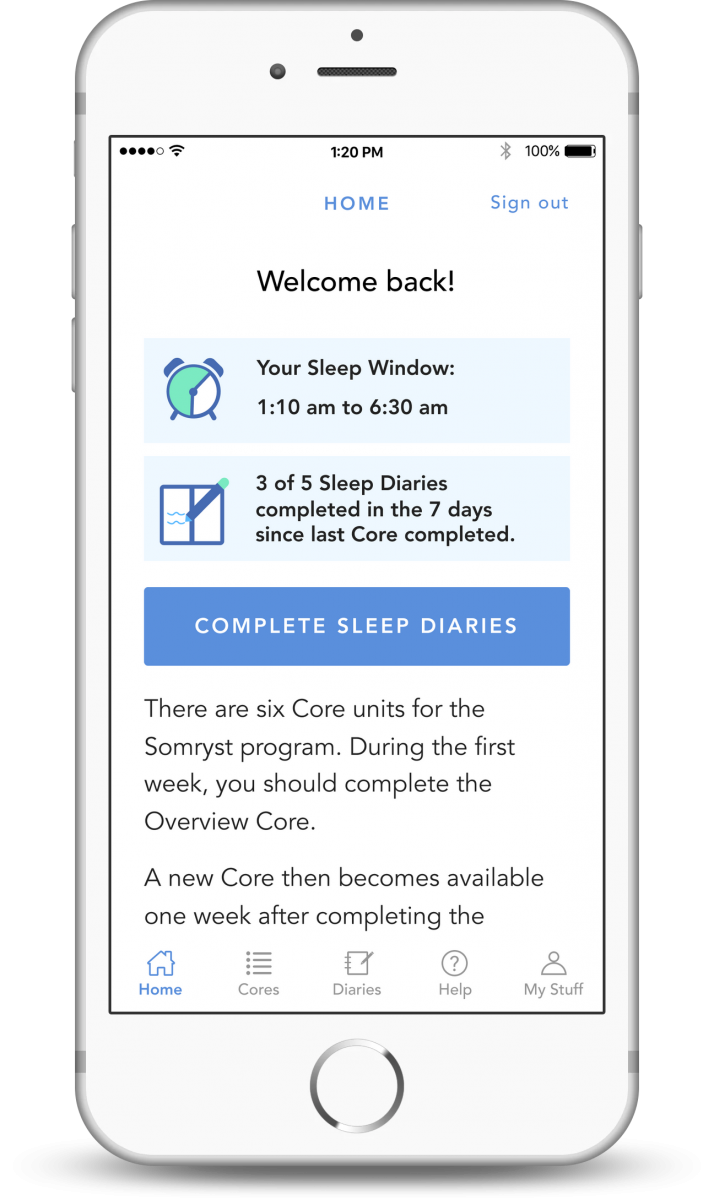
McCann described Somryst as a digital combination of cognitive behavioral therapy for insomnia (CBTi) and sleep restriction windows, both of which are personalized by an underlying algorithm to maximize their effectiveness for each patient.
According to the company, the Somryst submission is backed by two randomized controlled trials enrolling more than 1,400 adult patients with chronic insomnia or chronic insomnia with depression. The larger of these provided 1,100 adults with the treatment for nine weeks, and saw a significant reduction in insomnia and depression severity measurements compared to controls. These benefits persisted over an 18-month period, and also came with improvements to anxiety symptoms and suicidal ideation.
WHY IT MATTERS
If cleared, Somryst’s digital nature could address the scaling and dependency issues that current treatments for chronic insomnia and depression face, McCann said.
“CBTi is currently mandated as first line treatment for insomnia, but it is very very difficult for patients to receive in the real world because clinicians just aren’t sufficiently trained nor are they [incentivized] to provide face-to-face therapy of this degree of rigor,” he said. “So you can think of this as fitting into a paradigm for treating chronic insomnia as a first line treatment, and I think this is in very nice contrast to pharmacotherapies for insomnia. Things like zolpidem and benzodiazepines, which are better used in a short-term context, also have what is a habit-forming set of side effects and really don’t have the ability to provide a long-term clinical benefit as was demonstrated for Somryst.”
But along with the potential benefits of the treatment itself, Pear’s announcement serves as a progress report of sorts for the FDA’s experimental effort. The company is one of a handful that have already undergone the prerequisite quality inspections that are outlined in the Test Plan and Working Model. Now several months down the road, it is the first that has progressed to the point where its practices are being evaluated alongside a specific product submission.
“I think it’s important that products are not precertified; companies are precertified, and so really this is a framework where if a company is precertified it speaks to quality and quality of processes, and then that is a quality assessment that will ultimately be married to a evaluation of clinical study that demonstrates both safety and efficacy,” McCann said. “What I can say is that the quality inspection has taken place, and the FDA is reviewing our safety and efficacy dossier and looking at the two in their totality.”
Several stakeholders participating in the FDA’s pilot program or watching from afar have questioned whether this approach would inflict excessive, or for some startups inhibitory, burden on companies opening up their processes to regulator review. For Pear, however, that sort of quality demonstration is easy to justify when lives are on the line, and especially useful for a new modality looking to prove its place within the larger healthcare ecosystem.
“I would actually say that this is a level or rigor that is entirely appropriate for the treatment of severe medical conditions. I would specifically not use the word burden — I think this was actually a great opportunity for Pear to demonstrate what ‘good’ looks like in the creation of software to treat human disease,” McCann said. “I think that there’s a broader trend here, which is that there’s an acknowledgment that digital therapeutics and prescription digital therapeutics require evidence and a regulated path, and I believe that PreCert is really a helpful step in the right direction.”
THE LARGER TREND
Pear’s reSET was granted a De Novo clearance back in 2017, and in November of last year launched commercially with the help of Novartis. In the months to follow, Pear received the green light for reSET-O, brought in a $64 million Series C funding round and announced a new study targeting multiple sclerosis patients with depressive symptoms.
As for PreCert, the program appears to be chugging along since the FDA outlined and adopted its Working Model in January. Mid-May saw an update from the agency seeking new companies to test drive the framework and expanding the requirements from De Novo applications alone to 510(k)s as well. More recently, the regulator posted a mid-year update describing the pilot’s progress so far.
Focus on: The Future of Pharma
In the month of July, we'll take a closer look at the many answers to this question, as well as exploring what the changing face of pharma means for other healthcare stakeholders.

















