 Chronic disease management not only eats up upwards of 85 percent of US healthcare spending, it also accounts for seven out of 10 US deaths per year. So innovation in this sector is critical, but must take many forms, a panel of digital health companies said at Health 2.0.
Chronic disease management not only eats up upwards of 85 percent of US healthcare spending, it also accounts for seven out of 10 US deaths per year. So innovation in this sector is critical, but must take many forms, a panel of digital health companies said at Health 2.0.
“We can quote, all day, stats for chronic disease spending, and if we don’t work to reverse this trend, that amount will quadruple by 2023,” said moderator Dr. Bonnie Feldman.
Featuring representatives from Livongo, MyHealthTeams, Health Decision Technology, Wellness Layers and Sensely, the panel discussed the myriad ways they are working to reverse the financial and physical toll of chronic disease management. For some, it’s taking what has proven to be successful in fostering relationships: social media and dating sites.
“The way you use our site is a lot like Match.com,” said Eric Peacock, the CEO of chronic health social networking site MyHealthTeams.com. “We have engagements at Facebook levels.”
MyHealthTeams offers 23 networks, where visitors to the site select a condition, the type or stage and their top three symptoms. The visitors don’t have to have a condition themselves, but can be a family member, caregiver or friend of someone who is living with a chronic condition. Here, they can share their story with people who understand what they are going through, from treatment success or failures to just venting and being supportive of one another.
Unlike PatientsLikeMe, another social network for people with chronic conditions, this site isn’t trying to marry research with the patient engagement platform.
“PatientsLikeMe is trying to crowdsource trials for patients,” said Peacock. “We’re trying to host the party.”
Site members can also search terms such as certain medications or therapies. For example, on the Parkinson’s site, which is the largest network on MyHealthTeams, visitors shared a type of boxing that has been a beneficial workout in reducing some of their symptoms.
“These are things that patients might share with each other, but maybe not in the clinic,” said Peacock. “Sixty-four percent of these 18,000 people with Parkinson’s are active on the site every month, and we see similar patterns across all of our networks.”
George Reynolds of Health Decision Technologies shared Positive Link, his company’s network for people living with HIV. He said managing this particular condition carries an extra set of challenges.
“The US spends $38 billion on HIV, and it’s not enough,” he said. “We have good drug therapies and care, but if we can’t get them on treatment, we can’t help them. Linkage to care is really the problem.”
Positive Links is available to anyone with a smartphone, delivering personalized, interactive reminders of appointments or medication and a virtual support network. It targets both urban populations and those in rural, dispersed areas, where some people may be the only person in their community with HIV.
“There are some really tough demographics, and they need really strong social support,” Reynolds said. “On top of that, security is really important with HIV, you can’t necessarily comingle this with other services. We focus on a smaller community of trust.”
After social networks, the panel went into coaching platforms. Manny Hernandez of Livongo, which offers coaching for people living with diabetes, said his company’s method of mixing blood glucose monitoring with immediate actionable coaching has resulted in a positive change for their members.
“Among the members we surveyed, we have an improvement of one point on their HbA1c,” said Hernandez. “We have shown a reduction in low or high blood glucose episodes, which has resonated with clients, so they in turn show others, and the coaching network grows.”
Similar to Livongo’s approach, Wellness Layers offers a customized coaching platform called Coach Console. It consists of a patient-facing app and an administrative console for patient, coach and care team.
“So, coaching comes in a many flavors for chronic disease management, and it’s a critical part of supporting, giving knowledge and empathy to people, “ said Feldman. “Is this coaching all driven by technology, or are there people in the process?”
The panel said it’s a mix, that should start and stop based on what the patient needs. Since chronic conditions last a lifetime, the speakers posed the question of whether virtual, technology-enabled coaching was a better method for reaching patients than real humans, particularly as patients and coaches alike go through different stages of their lives.
“Something we have noticed in some autoimmune diseases like Crohn’s or colitis is patients will be on board with real coaching and taking medication, then they get to 18, they don’t want to deal with this stupid disease anymore; they want to go out and drink beer with friends and act normal,” said Peacock of MyHealthTeams. “Part of what we are doing is getting a lot of people onboard to talk about how you balance these things. You start this support early.”
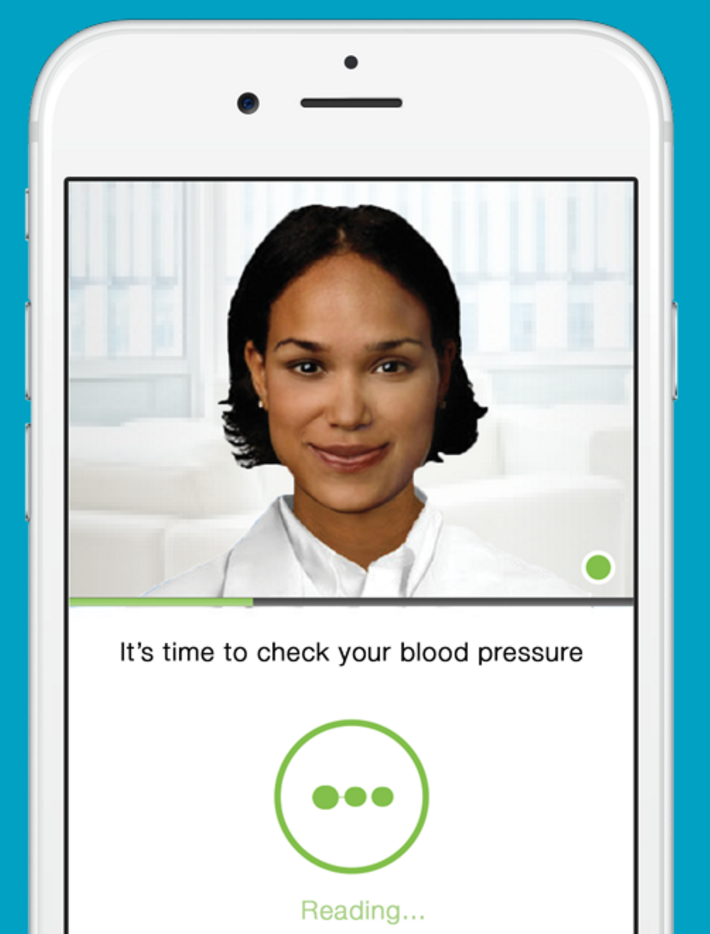
For Adam Odessky of Sensely, his AI-based coaching program was the most technologically-heavy on the panel. Demonstrating Molly, a lifelike avatar that conducts virtual visits on an app, Odessky explained that the virtual human brought an extra layer of coaching that texting or emailing doesn’t.
“The virtual health assistants provide three things: companionship and empathy, education, and remote monitoring,” he said, adding that there is also a telemedicine platform so users can interact directly with an actual flesh-and-blood human as well.
Sensely makes hundreds of avatars that are chosen based on what the patient prefers, and they are being used at a couple of hospitals around the US and UK. Odessky said engagement rate is high.
“The avatar-human approach is a hybrid, because either one isn’t the best,” he said. “You start engaging people early, and then you figure out what you need to be for them.”


















