 A new report on telemental health in Health Affairs shows that, among rural Medicare beneficiaries, use of telemedicine for mental health is growing quickly but inconsistently across the population. The piece is meant to provide perspectives for legislatures as they consider increasing Medicare coverage of telemedicine.
A new report on telemental health in Health Affairs shows that, among rural Medicare beneficiaries, use of telemedicine for mental health is growing quickly but inconsistently across the population. The piece is meant to provide perspectives for legislatures as they consider increasing Medicare coverage of telemedicine.
“We found that from 2004 to 2014 there was rapid growth nationwide in telemental health use among rural Medicare beneficiaries diagnosed with mental illness,” authors, led by Harvard healthcare policy professor Ateev Mehrotra, wrote in the report. “However, the use of telemental health within this population varied dramatically across states and was highly concentrated in terms of both who received that care and who provided it.”
Specifically, an analysis of claims data over the ten-year period showed an average growth rate of 45.1 percent per year for beneficiaries with any mental health condition and 49.3 percent per year for those with serious mental health conditions. In 2014, there were 5.3 telemental health visits per 100 beneficiaries with any condition and 11.8 visits per 100 beneficiaries with serious conditions.
Those who used telemedicine were more likely to be under 65, were more likely to have a disability that made them eligible for Medicare, and were generally worse off economically.
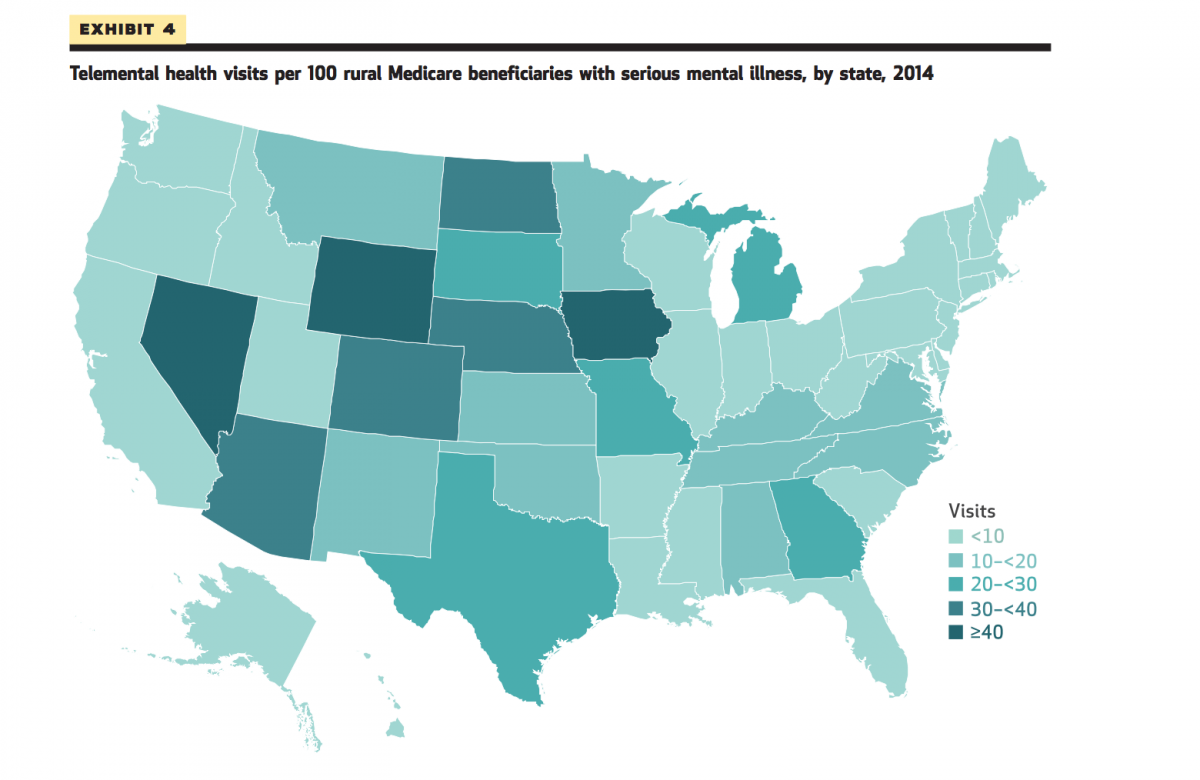
There was also a wide variation across states, with nine states having more than 25 visits per 100 beneficiaries with a serious condition and four states plus DC having no visits at all in the sample. Authors couldn’t fully account for the differences between states, but did say that states with telemedicine parity laws and states with an A rating from the American Telemedicine Association on their regulatory environment had significantly higher rates of use. Of course, the authors admit, this could also be at least partially a reporting bias, since doctors in states without parity laws might be less inclined to submit a claim for a telemedicine visit, and the research is based on claims data.
Who were patients visiting via telemedicine? Sixty-five point three visited psychiatrists, 19.9 consulted with nurse practitioners, and 8.8 percent spoke with clinical psychologists. The data was also heavily influenced by a relatively small number of doctors doing a lot of visits: according to the data, just 100 clinicians provided half of the 87,000 telemental health visits in the sample in 2014.
But what’s most concerning for the authors is that 87.3 percent of those who used telemental health also reported at least one in-person visit.
“Telemental health has been promoted as a way to extend mental health specialist care to patients without access to such care in their community, but we found that a relatively small fraction (less than 15 percent) of rural telemental health recipients received mental health specialty care only via telemental health,” the authors write. “Thus, telemental health appears to be complementing and supplementing in-person care. While this may improve the care these patients receive, telemental health use does not appear to be greatly expanding the number of rural beneficiaries who receive any mental health specialty care.”
If this sounds familiar, it should: Some of these same authors wrote another piece in Health Affairs earlier this year that raised a similar concern about direct-to-consumer telemedicine. When it comes to advising Congress on expansion of telemedicine coverage under Medicare, these worries about how telemedicine is used are an important part of figuring out whether it will really engender savings.
“Any payment policy for a new medical technology must find a balance between encouraging high-value care (where patients benefit clinically) and not encouraging low-value care (where there is little or no clinical benefit),” the study says. “With telemedicine, concerns about encouraging low-value care might be particularly salient because of its convenience.”













