 In a recent JMIR study, a team of researchers in Minnesota explored the potential of mobile health to reach people who sometimes fall through the cracks of the healthcare system. They found that a text message intervention could help Korean American women, a group that has one of the highest cervical cancer mortality rates in the United States, seek preventative screenings (Pap tests).
In a recent JMIR study, a team of researchers in Minnesota explored the potential of mobile health to reach people who sometimes fall through the cracks of the healthcare system. They found that a text message intervention could help Korean American women, a group that has one of the highest cervical cancer mortality rates in the United States, seek preventative screenings (Pap tests).
"A variety of structural and cultural factors act as barriers to screening for Korean American women," the authors write. "Structural obstacles include health access due to inadequate health insurance, expense, time constraints, and language limitations. Cultural barriers to cervical cancer screening encompass lack of knowledge regarding cervical cancer and cervical cancer screening, a wrongly held belief that screening is unnecessary in the absence of symptoms or at young ages, cultural modesty or embarrassment, lack of culturally appropriate health care providers, and fear of receiving negative screening results."
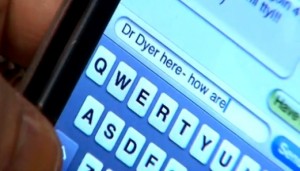
Researchers designed a text message based intervention for a study group of 30 Korean American women, 90 percent of whom had been living in the United States for less than 9 years and nearly two-thirds of whom had a family history of cancer. Based on a screening conducted ahead of time, women received messages tailored to their specific needs; for instance, a woman who had scored high on a pre-test scale for cultural embarrassment might receive the message “We understand it is a bit embarrassing to get it done. But do it for you! Your happy cervix will appreciate it!” in addition to the other messaging. Participants received messages for seven days, and many of them were interactive, prompting responses from the participants.
Results were mixed. A week after the intervention, participants were generally more knowledgable about cervical cancer and the importance of screening. Significant differences were observed in general knowledge, knowledge of risk factors, and knowledge about and attitudes toward the Pap test. But when asked whether they planned to get a screening in 1 year, 3 months, 1 month, or not at all, the increase wasn't statistically significant, though this could be owing partly to the small sample size. At a three month follow-up, just seven of the 30 women had actually gone in to get screened for cervical cancer.
Nonetheless, researchers are hoping to follow up the study with a larger RCT, possibly modifying the experiment design to deliver the messages over a shorter time or to incorporate a smartphone app.
"Given the widespread use of mobile phones (98 percent) and smartphones (83 percent) among young adults, a mobile phone-based health intervention could be a cost-effective method of reaching hard-to-reach populations with tailored, individual messages that cover broad content areas and overcome restrictions to place and time of delivery," they wrote. "Our developed model could be expanded for delivery to different age groups of Korean American women to promote additional types of cancer screening, such as colonoscopy or mammogram. It could also be used with other underserved minority groups. Vietnamese, Hmong, and Laotian American women face similar barriers to cancer screening and report high cervical cancer incidence and mortality. It is likely that these populations may also benefit from a similarly tailored intervention approach."














