 HealthCrowd has raised $2.1 million to expand the scope of its patient outreach business in several different ways. Startup Capital Ventures, Herlitz Capital, Healthy Ventures, Band of Angels, Berkeley Angel Network, and 37 Angels all participated in the seed round.
HealthCrowd has raised $2.1 million to expand the scope of its patient outreach business in several different ways. Startup Capital Ventures, Herlitz Capital, Healthy Ventures, Band of Angels, Berkeley Angel Network, and 37 Angels all participated in the seed round.
"Most people in the industry, as well as the Medicaid space, know us as the text messaging platform," CEO Bing Doh told MobiHealthNews. "Not exactly a bad thing, but it’s not what we originally set out to do. We found an opportunity and were able to fill a need and really demonstrate results. From the get-go we always wanted to be a communications platform."
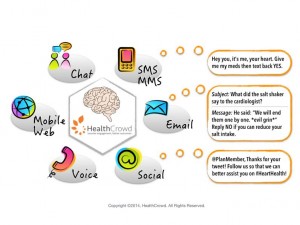
Though it's what they're best known for, text messaging is just one automated modality HealthCrowd uses to reach out to patients, along with automated phone calls, nanosites, chats, email, and mail -- all automated to allow for scale in large populations. What's novel about the platform, Doh said, isn't just that it encompasses so many ways to reach patients but that it combines them in an intelligent way.
"Any smart platform should be learning from every single interaction that they’ve ever had with a member and with a population," she said. "If I’m doing my second robocall, I’m looking back in the past to see this member has never picked up the phone, or they have picked up the phone but it was on a weekday, but it was between 10-12 o' clock. Instead of blindly initiating another blast to the whole population, we should be smart enough to know when to actually call that particular person."
Moving beyond the text message is one way HealthCrowd is expanding its business. It's also looking to expand its customers beyond Medicaid to other parts of it's payer customers' business books. And finally, HealthCrowd wants to help customers with all parts of their business, not just the clinical side.
"The reason we moved away from being an engagement company is because there are so many other use cases besides the clinical realm," she said. "Getting people to get their shots and take their medications and go to their primary care appointments, we’re really good at that, but that’s only one piece of a members’ experience, it’s not everything. And if you think about the organization, yeah sure, they want people to take all these healthy actions but that’s not the only thing they care about."
They want to see customers' member services, grievances and appeals, marketing departments, and legal departments use their tools as well. In addition, changing times are necessitating an increasing focus on legal protection as a value proposition.
"The amount of automated digital outreach in our lives has increased at an exponential pace over the last five years," Doh said. "For example, we get emails, text messages, phone calls, from the restaurant we’re trying to get seated at, your airline, your bank, it’s a lot and it’s grown at a very rapid pace. That means that if I’m becoming desensitized and now my health plan is trying to reach me about a million and one different things, you have to figure out, one, how to cut through the clutter, but, two, how do you protect yourself from getting sued? There have been many, many lawsuits over the past several years about members and patients being contacted by their health plan and even by their provider and it was unsolicited. So we have to make sure we’re protecting our providers and keeping them out of harm’s way because these fines are in the millions."











