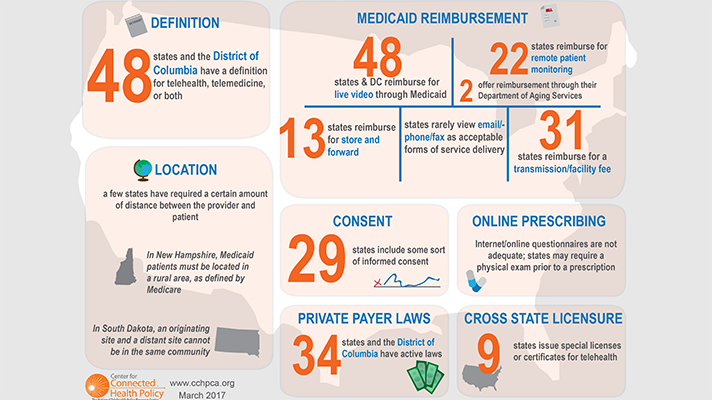
 The Center for Connected Health Policy has released the fifth edition of its State Telehealth Laws and Reimbursement Policies Report. CCHP uncovered many notable findings in the new report. Perhaps chief among those: 48 states and Washington, D.C., provide reimbursement for some form of live video in Medicaid fee-for-service.
The Center for Connected Health Policy has released the fifth edition of its State Telehealth Laws and Reimbursement Policies Report. CCHP uncovered many notable findings in the new report. Perhaps chief among those: 48 states and Washington, D.C., provide reimbursement for some form of live video in Medicaid fee-for-service.
Specifically, 13 states reimburse for store-and-forward delivered services in Medicaid; states that only provide reimbursement for teleradiology were not counted in this number. Twenty-two states reimburse in Medicaid for remote patient monitoring.
The report also found that 31 states provide a transmission and/or facility fee. Six states have geographic/rural restrictions. And 23 states limit Medicaid reimbursement to a specific list of facilities.
“While many states are beginning to expand telehealth reimbursement, others continue to restrict and place limitations on telehealth delivered services,” CCHP said in the report. “Although each state’s laws, regulations and Medicaid program policies differ significantly, certain trends are evident when examining the various policies.”
When it comes to private payer reimbursement, 35 jurisdictions have laws that govern reimbursement of telehealth, the report found. This number has remained constant since CCHP’s August 2016 update, although some states have made modifications to their private payer law. Some laws require reimbursement be equal to in-person coverage; however, not all laws mandate reimbursement.
Looking to the future, CCHP noted that 44 states have already introduced some 200 pieces of telehealth-related legislation addressing reimbursement for both private payers and government agencies.
“Other noteworthy trends include the addition of the home as an eligible originating site in some states, and the inclusion of teledentistry as a speciality qualifying for Medicaid reimbursement and/or required to be reimbursed by private insurers,” CCHP said.


















