 Telemedicine has been around for a number of years, but it's not yet an everyday channel for patients to receive care. A panel of providers and vendors sat down at the Partners HealthCare Connected Health Symposium to discuss the question of what it would take to get telemedicine into the mainstream.
Telemedicine has been around for a number of years, but it's not yet an everyday channel for patients to receive care. A panel of providers and vendors sat down at the Partners HealthCare Connected Health Symposium to discuss the question of what it would take to get telemedicine into the mainstream.
The panel, moderated by Harvard heart surgeon Lawrence Cohn, included American Well CEO Dr. Roy Schoenberg, Mercy Health CFO Shannon Sock, Wellpoint Chief Strategy Officer Dr. Martin Silverstein, and Dr. Neil Evans, Co-Director of Connected Health at the Department of Veterans Affairs.
"Like any new product category, you need to have awareness, you need to have a value proposition, and make sure the average patient has access to this as a benefit," Silverstein said. "But a lot of employees have access to this as a benefit, some with no copay at all, and they’re still not using it. I think it has to do with awareness. They have to understand the value proposition and they have to develop a confidence that this is good medicine. And I’m not sure there’s enough consensus on what good practices are. It needs to become more mainstream and it needs to become a more visible part of the healthcare ecosystem and [then] they'll have the confidence."
The panel did agree that regulatory barriers like state licensing laws and lack of reimbursement were holding telemedicine back. But most agreed that those factors were not insurmountable.
"I would say the parallel to this is the [retail] clinic," Silverstein added. "[Retail] clinic adoption in many markets took quite a while. But when there was a awareness through advertising, covered benefits through insurance, and word of mouth, people started to get comfortable."
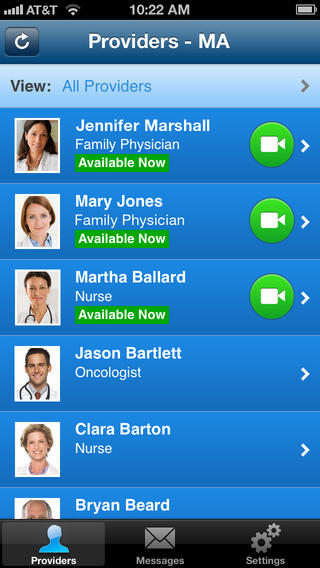
Schoenberg said that a big lesson in what would drive adoption came from American Well's own experience launching its mobile app last year.
"We’ve been offering telehealth services in a variety of different ways through the web to patient populations," he said. "And then just about a year ago we turned on access through your mobile device, and we’re seeing a hundredfold increase. ... The reality is how people use telehealth has completely changed because of a single thing they have in their pocket. Sometimes the solution is not having flashier statements and better communication, it’s just by making that little tweak that makes it part of the fabric of people’s lives."
Evans, whose organization has been a pioneer in the use of telemedicine, said the best way to get patients to adopt technology is a plea from someone they trust: their doctor.
"Healthcare is about relationships that are built on trust," he said. "When patients are invited to participate in telemedicine, telehealth, or connected health by their personal provider, adoption increases tremendously."
Mercy Health's Sock, however, dissented from the panel on where the onus for increasing adoption lies.
"I don’t think it’s a consumer uptake issue at all," he said. "We’re seeing tremendous uptake in the tools that we provide. Today in Mercy we have over 600,000 active users of our MyMercy platform. We offer structured eVisits that people pay for routinely. It’s not a consumer or patient issue, and I would suggest it’s not a payer issue either. I think it’s a provider issue. When I'm talking to my peers on the provider side I’m trying to encourage them to view it in three dimensions: There’s adequate evidence that telemedicine provides a positive clinical platform, there's increasing evidence it drives efficiency, and -- and this is the part I don't think there's enough of -- viewing it as a strategic asset. When you put that mindset on, you’re thinking about how you grow your organization, how you increase the size of your patient populations."
Mercy Health is about to build a new telemedicine center, Sock said, that will handle everything from an eICU to virtual primary care. He's confident the industry will catch up.
"As a large provider, I've heard lots of conversations about leadership and adoption and what will be the tipping point for adoption," he said. "We started our journey about 10 years ago and made the decision that we’re not going to wait for the industry, we’re not going to wait for reimbursement, so we’ve invested heavily in this capability."












