 Arkansas, which lags behind the rest of the country in regards to telemedicine, approved one medical board rule to expand telehealth services in the state, but rejected a second that would change requirements for doctors’ use of telemedicine, Arkansas’ KUAR radio reports. While the first rule allows doctors and patients to establish a relationship via audiovisual technology, the lack of a decision on the second keeps the status quo of not allowing non-video companies like Teladoc to see patients in the state.
Arkansas, which lags behind the rest of the country in regards to telemedicine, approved one medical board rule to expand telehealth services in the state, but rejected a second that would change requirements for doctors’ use of telemedicine, Arkansas’ KUAR radio reports. While the first rule allows doctors and patients to establish a relationship via audiovisual technology, the lack of a decision on the second keeps the status quo of not allowing non-video companies like Teladoc to see patients in the state.
Talk Business & Politics reports the Arkansas Rules and Regulations Subcomittee of the Arkansas Legislative Council approved the State Medical Board’s amendment of Regulation 2.8, which allows the use of real-time audiovisual technology for first time visits between a doctor and patient, rather than requiring an in-person visit. But Regulation 38, which defines requirements for a doctor to practice telemedicine (namely, where they are located), remains unresolved due to disagreements over the definition of store and forward technology.
Claudia Tucker, Teladoc’s vice president of government affairs, said “store and forward” has nothing to do with any type of loophole that Teladoc or others may be seeking, and said interactive audio (which has been used in nearly all telemedicine bills introduced recently in state legislatures), is meant to include data and information that supplements live audio.
“This isn’t a Teladoc issue; this is an industry issue,” Tucker told MobiHealthNews. “While Arkansas has actually done very well with highly specialized telemedicine offerings like neonatal care and stroke treatment, it’s behind on the basics, like non-emergency doctor visits.”
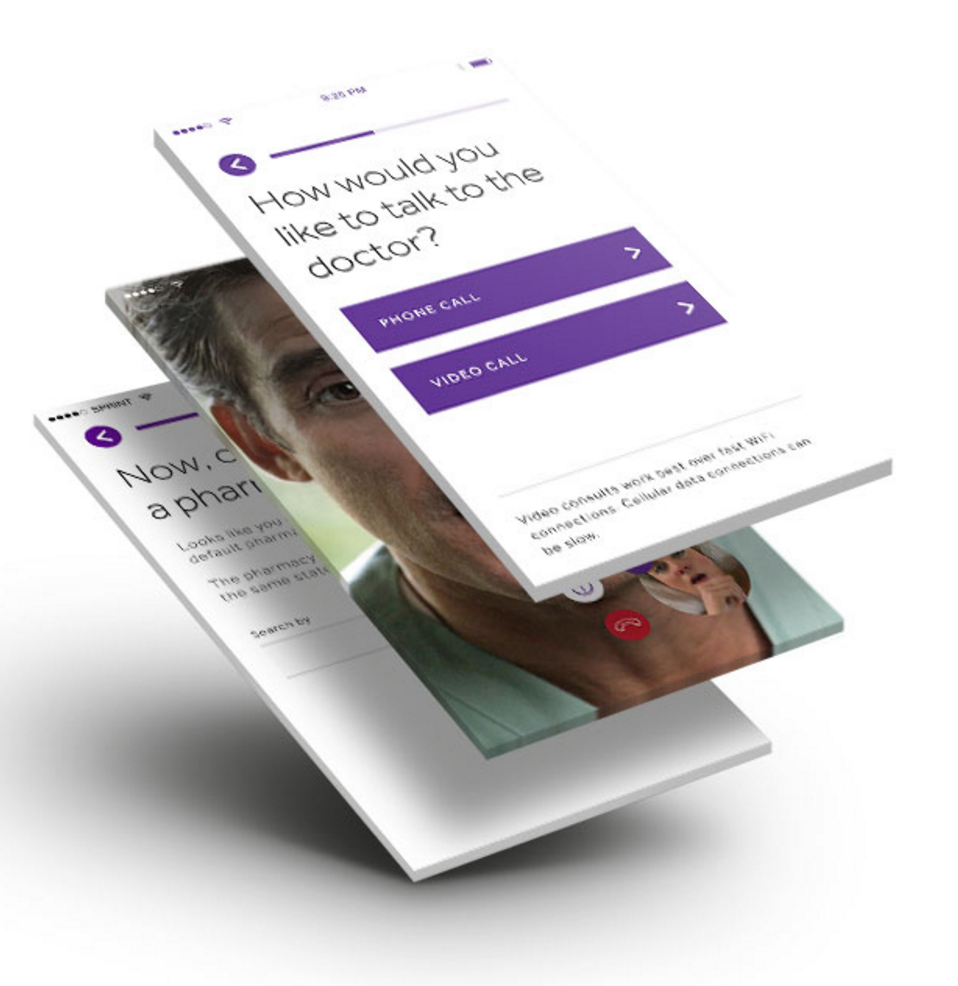
Through several large companies, including Teladoc and American Well, patients can contact doctors they have never met in person by using either video device of a phone, but Arkansas has attempted to put a stop to the perceived loophole in the phone call relationship. When regulation 38 was originally approved, an amendment was added at the last minute that caused concern, wherein the definition of store and forward was changed from allowing medical history and personal data to excluding it.
Tucker said it seemed like an overreach by the board that restricts what is currently offered in most states.
“I’ve gone all over the country. There are 13 states that have adopted store and forward language similar to this. They want to include data. Arkansas is out there by themselves,” she said.
Arkansas, which the American Telemedicine Association ranks last in the nation in telemedicine practices, doesn’t allow companies like Teladoc or American Well to see patients. While other states are figuring out various methods of expanding telemedicine, Arkansas, like Texas, is still tussling with definitions of proper doctor-patient relationship protocols. A group called the Texas eHealth Alliance is now circulating an updated version of its draft rules it submitted last month.
Politico found that about a dozen states in the last two years have authorized “interactive audio” or audio using store-and-forward technology in their statutory definitions of telemedicine. Under this definition, doctors can treat patients for the first time through telephone calls so long as the patient has filled out a medical history questionnaire prior to the call. Arkansas doesn’t like this.
“My guess is that very few if any legislators really understand that they’ve created that loophole,” Arkansas Medical Society attorney David Ivers told Politico. “On the surface, that doesn’t sound very concerning. The problem is you have telemedicine vendors, or at least one, who claims that online medical questionnaire is store-and-forward technology.”
As the Arkansas Medical Society Executive Vice President David Wroten told Politico, phone medical visits for first-time patients are “just not good medicine.”
But Tucker said this perception of a loophole is off-target. Additionally, Tucker said, employers all over the state want telemedicine. The CDC ranks Arkansas as sixth worse in the nation on the number of primary care physicians per capita.
“Every single county is an underserved county,” Tucker said. “Employers are making a strong statement that they want this benefit. Consumer patients are educated about this. They are not passive recipients of healthcare. My question is, why shouldn’t they have access? Why, when a doctor gets involved with patients, would you not want them to have every piece of information?”














