 The National Institute of Diabetes and Digestive and Kidney Diseases, a part of the National Institutes of Health, has given out $41 milion in grants to four studies that will hopefully make the artificial pancreas – a long-sought, fully automated, closed-loop system for insulin regulation – a reality. Two of the studies are underway and two more are slotted to begin recruiting in the next two years.
The National Institute of Diabetes and Digestive and Kidney Diseases, a part of the National Institutes of Health, has given out $41 milion in grants to four studies that will hopefully make the artificial pancreas – a long-sought, fully automated, closed-loop system for insulin regulation – a reality. Two of the studies are underway and two more are slotted to begin recruiting in the next two years.
“Managing type 1 diabetes currently requires a constant juggling act between checking blood glucose levels frequently and delivering just the right amount of insulin while taking into account meals, physical activity, and other aspects of daily life, where a missed or wrong delivery could lead to potential complications,” Dr. Andrew Bremer, the NIDDK program official overseeing the studies, said in a statement. “Unifying the management of type 1 diabetes into a single, integrated system could lift so much of that burden.”
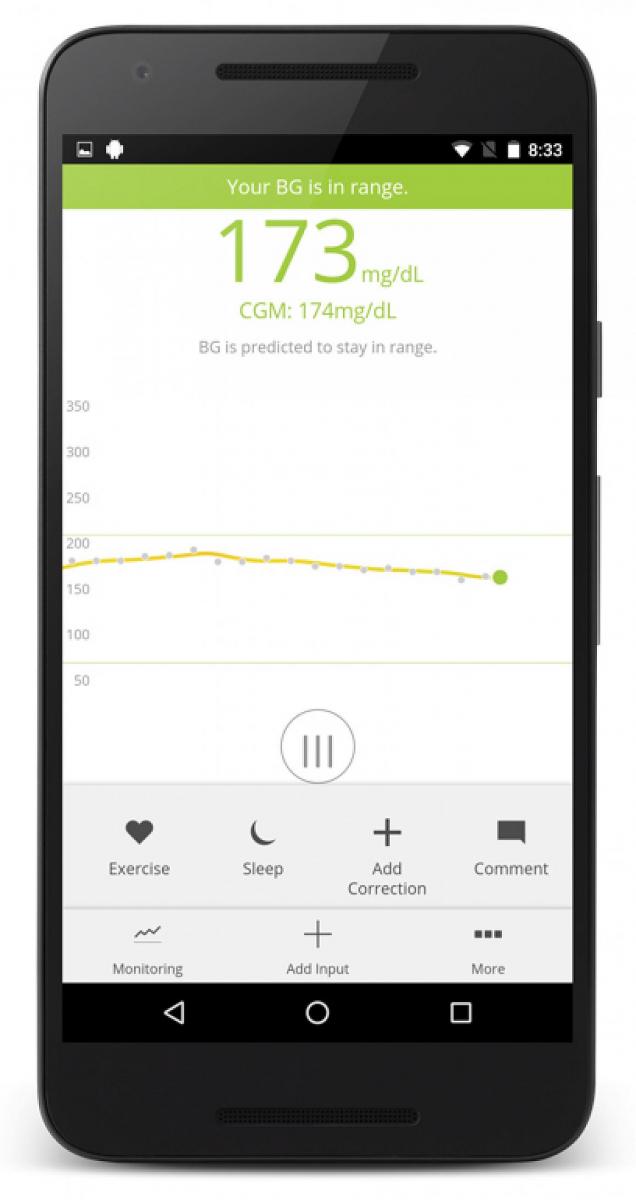
A long-sought dream of diabetes technologists, an artificial pancreas would combine the functionality of an automated insulin pump and a continuous glucose monitor, automatically calculating dosages and delivering insulin based on readings from the CGM -- in essence replicating the behavior of a normally-functioning human pancreas, which regulates insulin in people without diabetes.
The four studies all vary from previous artificial pancreas studies in a few key ways. For one thing, they will each have 100 or more participants. For another, while previous studies looked at geographically co-located cohorts at summer camps for youth with diabetes or hotels near the study site, these studies will be conducted at multiple sites, remotely, allowing researchers to test the systems in natural, real-life contexts.
The studies will hopefully provide the data the FDA needs to clear a fully closed-loop system. Last year the FDA cleared Medtronic's artificial pancreas, but that was a hybrid system that still required patients to manually adjust insulin intake at mealtimes.
We wrote about one of the four studies when it began enrollment last year. The International Diabetes Closed Loop trial at the University of Virginia aims to enroll 240 adults with type 1 diabetes. The participants will come from 10 different clinical sites throughout the world – including Mount Sinai Hospital in New York, Stanford University Hospital and the Mayo Clinic in the United States, as well as medical centers in France, Italy and the Netherlands. A Tandem insulin pump and Dexcom G5 sensor will be included as part of a blood glucose control system that combines the devices with a smartphone running TypeZero’s closed loop algorithm app inControl.
The other study that has already begun recruiting is led by Dr. Roman Hovorka of the University of Cambridge in England. The 130-person study of teenagers, which looks at a system called FlorenceM using an Android smartphone and Medtronic devices, will be conducted at sites in California, Colorado, Connecticut, Minnesota, and two sites in the United Kingdom.
A third study is scheduled to begin recruiting this year. It's led by researchers from the International Diabetes Center in Minneapolis and the Moshe Phillip of Schneider Children's Medical Center in Petah Tikva, Israel and will include 100 youths at sites in California, Connecticut, Florida, Massachusetts and Minnesota and abroad in Germany, Israel and Slovenia. It will compare the FDA-cleared hybrid system with a next-generation version of that system from Medtronic.
Finally, the fourth study will kick off in 2018, led by researchers in Boston from Massachusetts General Hospital and Boston University. The six-month study is a little different from the others -- it looks at a “bionic pancreas” system, with a dual-chamber pump to deliver both insulin and its counteracting hormone, glucagon, using tested algorithms for automated dual-hormone delivery. The study will include two sites in California and one each in Massachusetts, Michigan, Missouri, North Carolina, Ohio and Washington.
“For many people with type 1 diabetes, the realization of a successful, fully automated artificial pancreas is a dearly held dream. It signifies a life freer from nightly wake-up calls to check blood glucose or deliver insulin, a life freer from dangerous swings of blood glucose,” said NIDDK Director Dr. Griffin P. Rodgers. “Nearly 100 years since the discovery of insulin, a successful artificial pancreas would mark another huge step toward better health for people with type 1 diabetes.”
















