A newly published randomized controlled trial study suggests that using mobile devices for self-tracking and feedback could be a cost-effective way to scale successful weight loss programs that include a face-to-face component.
The study, published in the Journal of the American Medical Association and completed in September 2010 at a Midwestern Veterans Affairs hospital, split a group of 70 older, mostly male veterans into two groups. Both groups attended biweekly MOVE! sessions for 6 months, but one group was issued Palm Pilots during that time and instructed on how to record their food intake, weight, and physical activity. They uploaded the data to a server where it could be accessed by coaches, who phoned them every two weeks for about 15 minutes to talk about their data and progress toward a 5 percent weight loss goal. After the six months were over, participants continued to record and transmit data, but less frequently, and coaches only followed up if participants failed to submit.
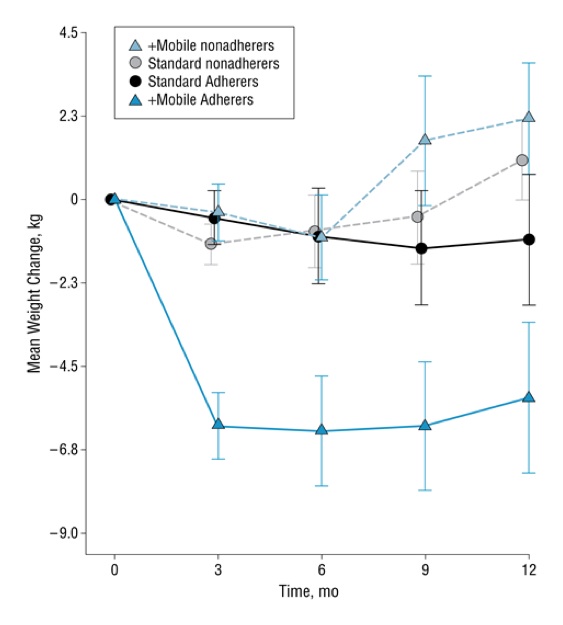
At every benchmark (three, six, nine, and 12 months), a larger percentage of the mobile intervention group had achieved the 5 percent goal than the standard group. At three months, 36.7 percent of the mobile users had met their goal, compared to none of the participants in the standard group. After 12 months, 29.6 percent in the mobile group had met the goal, compared with 14.8 percent in the standard group.
"The current results are, to our knowledge, the first to demonstrate that use of a mobile technology system and remote coaching can significantly augment weight loss and maintenance when added to an existing standard-of-care obesity treatment program," the authors write in the study. Though other interventions have been done with PDAs, they wrote, they have tended to also include intensive in-person treatment sessions. This study demonstrates that a mobile intervention can be a substitute for expensive, in-person sessions -- an important finding for those looking to mobile health as a solution to scalability problems with proven obesity treatments.
"In general, greater weight loss [12.5 - 19.4 lbs] occurs when technology is combined with weekly in-person contact," the study says. "However, because in-person interventionist contact is the most expensive treatment component to provide and the most burdensome to access, we substituted brief, regularly scheduled telephone coaching to which coaches came prepared by having reviewed participants' transmitted, analyzed data. Results suggest that connective technology, like that used in the current study, can allow telephone contact to substitute efficiently for face-to-face time."
Dr. Bonnie Spring of the Northwestern University Feinberg School of Medicine was the lead author of the study. She spoke at the mHealth Summit last week, using this data as an example of how RCT results are relevant in mobile health even when a lot of time has passed since the study was done.
"Even homely, not very attractive apps can be effective when they integrate valid behavior change strategies," she said. She said using the Palm Pilots, and teaching elderly seniors to enter their data and "hotsync" it with their personal computers, was somewhat frustrating. But the intervention was effective, she said, and translating the lessons learned to newer devices like smartphones and wireless activity trackers isn't hard to do.