 Last week Boston-based American Well made its telehealth service available as a direct-to-consumer offering. Now anyone with a camera-equipped smartphone, tablet, or computer can conduct a video visit with a physician for $49 -- assuming you live in a state that doesn't prohibit it. That means those in Texas, Louisiana, Alaska, Alabama and Oklahoma will have to wait until their state's representatives change policies.
Last week Boston-based American Well made its telehealth service available as a direct-to-consumer offering. Now anyone with a camera-equipped smartphone, tablet, or computer can conduct a video visit with a physician for $49 -- assuming you live in a state that doesn't prohibit it. That means those in Texas, Louisiana, Alaska, Alabama and Oklahoma will have to wait until their state's representatives change policies.
Up until now American Well has offered its web-based, video visit platform through insurance companies like UnitedHealth Group and WellPoint as well as some forward-thinking providers. In mid-2008 the company got its start with its first deal: Hawaii Medical Service Association (HMSA), a member of the Blue Cross Blue Shield Association. It has added many since. After five years of working exclusively through other healthcare organizations, the direct-to-consumer play is a big move for the company.
What's happened since 2008, is that telehealth is no longer a notion of an "academic novelty" but is rather "becoming bread and butter" for healthcare, American Well CEO Dr. Roy Schoenberg told MobiHealthNews. "It's now a valid channel for care delivery."
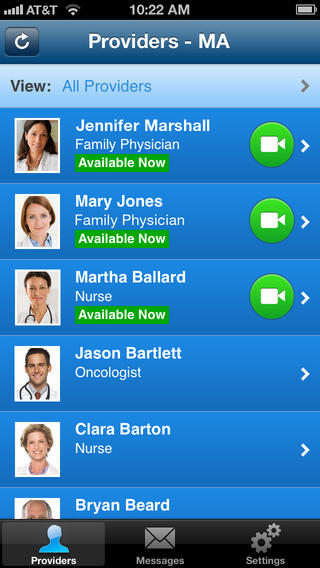
American Well launched iOS and Android apps as part of the DTC launch. Here's how the app works from the patient's view:
Once the app is downloaded the registration process fairly simple. The patient must first agree to the terms of service, then create a six digit numerical pin code. The third screen is a basic name, DOB, email, state, and gender form as well as a few optional fields to fill in health insurance information in case your insurance company covers video visits. On the fourth screen a list of available physicians and other healthcare providers (like dietitians) pops up and shows which are available right now. After selecting a medical professional a new screen displays the price (i.e. $49 without insurance) as well as the provider's educational background, languages spoken, and years of experience. By clicking "Talk Now" the app then asks for specific information about the reason for the visit, asks the patient to agree to the terms of use of the online pharmacy, and for a follow-up phone number. Finally, it asks where the patient might have gone if they hadn't chosen to use American Well. In the next to last step it asks for credit card information before connecting the patient with their chosen doctor.
"The end experience is really simple and trivial," Schoenberg said. "You hit something on your mobile phone, see a list of physicians, and hit connect, but a tremendous amount of work went into make this a proper extension of good healthcare."
Schoenberg said that American Well has more than 600 physicians in its network across those 44 states.
The majority of those states -- about 28 -- are "completely green", according to Schoenberg, because they allow the physician to use their own discretion as to what they can prescribe via virtual visits. Other states limit it to just antibiotics or medications for rashes, he said, but there is a spectrum.
American Well's platform has been largely used for primary care issues like the flu, rashes, headaches, migraines, UTIs, bronchitis, pneumonias, and pediatric issues, Schoenberg said. Increasingly more people with chronic conditions are using the video visits to check-in on a particular symptom to see if it is something they can take care of on their own with the "arsenal of medications" they already have at home, or if they should visit a healthcare facility, Schoenberg said.
"Healthcare is an industry that moves at a glacial pace usually, we are seeing this move forward at the pace of consumer technology, which is much, much faster," he said. "In the last 20 years people thought that healthcare would change because of electronic medical records, but this is the technology that will change healthcare in the next decade. And it won't be the same within the next year or two."




















